How Claims Processing Impacts Healthcare Providers
Claims processing is the heartbeat of a healthcare provider’s financial operations. It’s the process of submitting, reviewing, and receiving payment for medical services rendered — and when it’s not handled efficiently, the ripple effects can impact every aspect of a practice.
Unfortunately, many providers still experience issues like claim denials, payment delays, and underpayments. These inefficiencies don’t just cause financial stress — they reduce the time and resources available for patient care.
What Is Claims Processing in Healthcare?
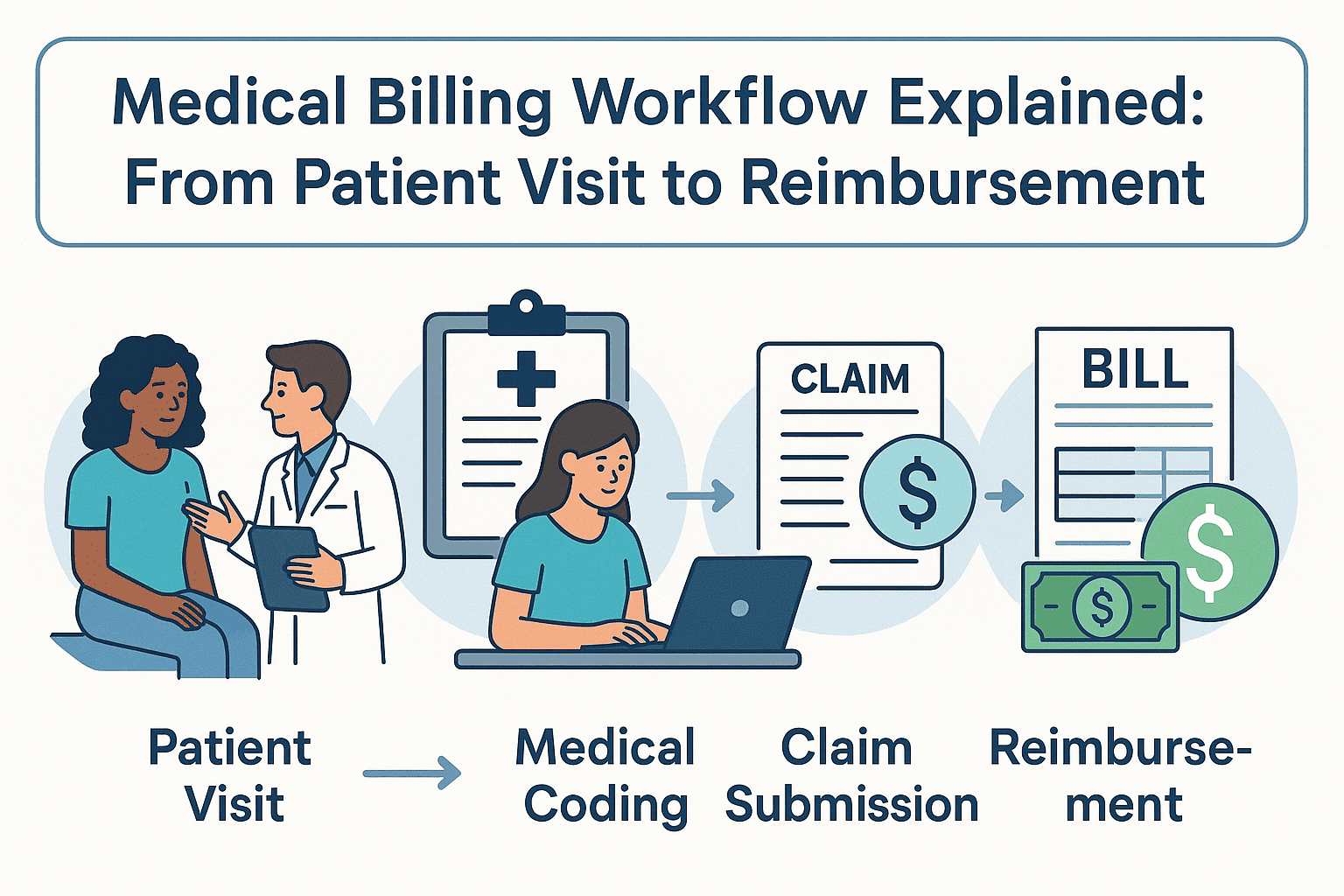
Claims processing involves translating medical services into billing codes, submitting claims to insurance payers, and following up on payments. The process typically includes:
- Verifying patient insurance and eligibility
- Coding services using CPT/ICD codes
- Submitting claims electronically
- Resolving denials or rejections
- Posting payments and reconciling accounts
Every step must be precise. A single mistake can mean a denied claim or lost revenue.
Common Challenges in Claims Management
Even experienced billing teams face frequent obstacles:
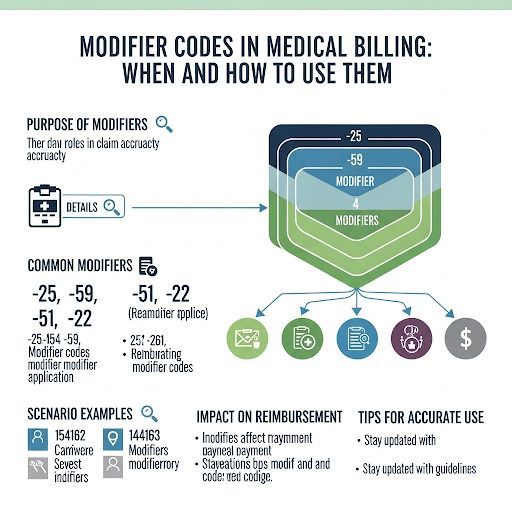
- Coding errors leading to denials
- Missing documentation
- Inaccurate patient data
- Lack of follow-up on unpaid claims
- Constantly changing payer rules
These issues often require providers to spend valuable hours on rework, follow-up calls, and appeals — all of which strain staff and reduce efficiency.
The Financial Toll of Inefficient Claims Processing
Delayed or denied claims don’t just slow down payments — they jeopardize a practice’s cash flow. Consider that most practices operate on thin margins. Every day a claim goes unpaid increases the risk of revenue loss.
Outsourcing claims processing to Medical Billing Outsourcing Companies in USA can relieve these burdens by bringing in specialized expertise and scalable systems that ensure faster turnaround times.
Why Accurate Claims Processing Matters
Accurate and timely claims processing leads to:
- Fewer denials and rejections
- Improved cash flow
- Less administrative overhead
- Better relationships with patients and insurers
It also reduces the time between service delivery and reimbursement — keeping your revenue cycle moving.
How California Providers Benefit from Expert Billing Support
In a competitive and high-volume market like California, providers often turn to Medical Billing Services California to help streamline claims management. These services ensure accuracy, compliance, and consistency — all critical for avoiding delays and denials.
Credentialing and Its Role in Claims Success
Credentialing may not seem directly connected to claims processing, but it's essential. Without verified credentials, insurance companies may reject claims outright. Partnering with reliable Credentialing Services California ensures your providers are approved to bill payers and that claims get accepted on the first submission.
Why Choose Valley Medical Billing Services
At Valley Medical Billing Services, we understand the intricacies of claims processing and the pressure providers face. Our certified billing professionals stay current with payer guidelines and compliance rules to ensure your claims are submitted accurately and on time.
We offer:
- End-to-end claims management
- Denial resolution
- Payment posting and reconciliation
- Credentialing and insurance verification
- A/R follow-up and recovery
We don’t just process claims — we help you get paid faster, with fewer headaches.
Spend your time making money, not trying to bill for it. Schedule a free consultation with Valley Medical Billing Services to learn how we can help your practice thrive.