Explanation of Benefits (EOB): What It Really Means
Introduction: Why EOBs Confuse So Many Patients
If you’ve ever opened a letter from your insurance company after a doctor’s visit and thought, “Wait, I still have to pay this?”, you’re not alone. This document — called an
Explanation of Benefits (EOB) — is one of the most misunderstood parts of the medical billing process.
In this guide, we’ll break down what an EOB really means, why it matters, and how small practices can use this tool to improve transparency with patients.
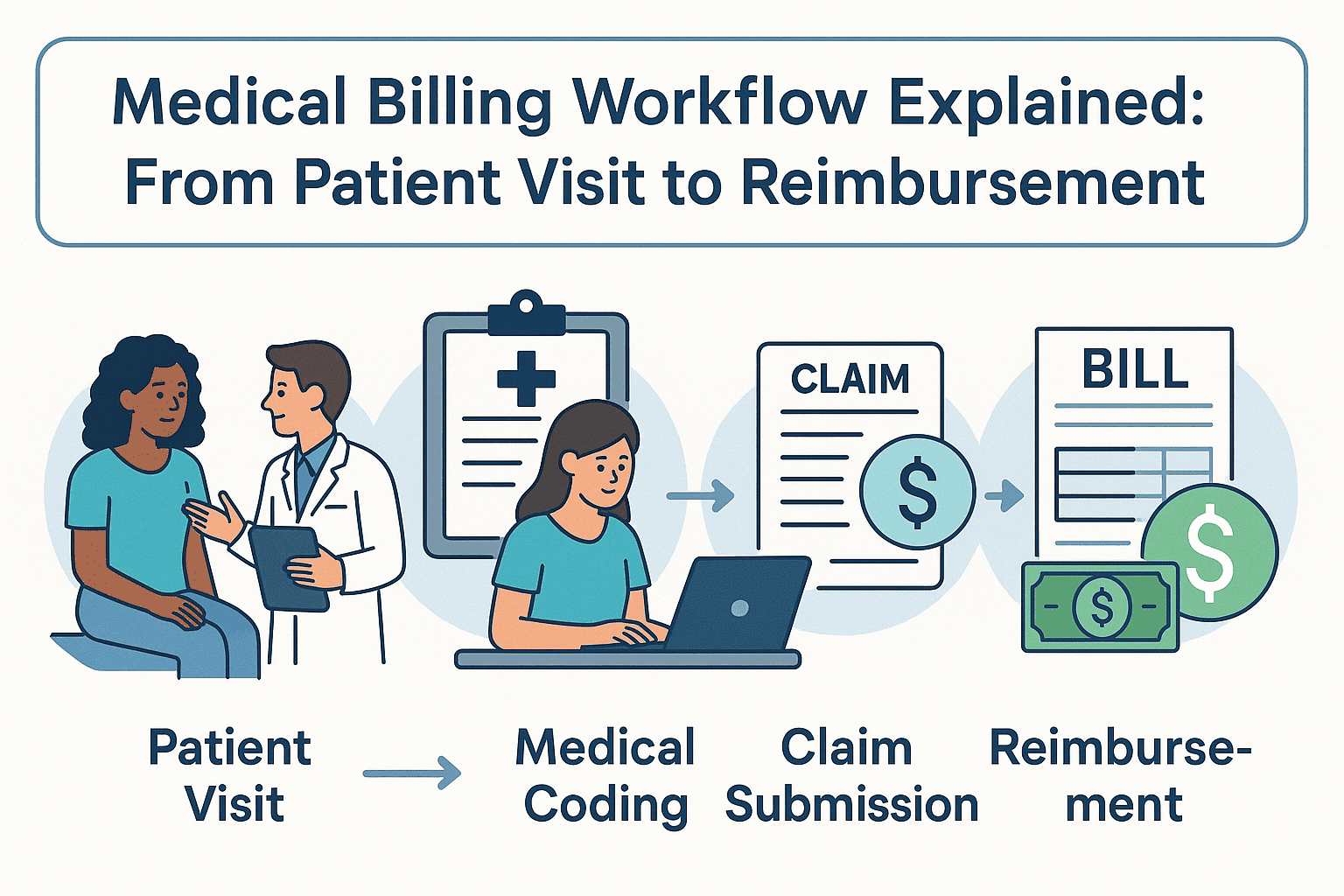
What Is an Explanation of Benefits (EOB)?
An EOB is a statement sent by your health insurance provider after a healthcare service is processed.
It
is not a bill — it’s an informational summary showing:
- The services performed
- What your provider charged
- What your insurance covered
- Any amount you may owe to the provider
Key Parts of an EOB
While EOB layouts vary by insurance company, most include the following sections:
Section
What It Tells You
Patient Information
Name, date of service, and provider details
Services Provided
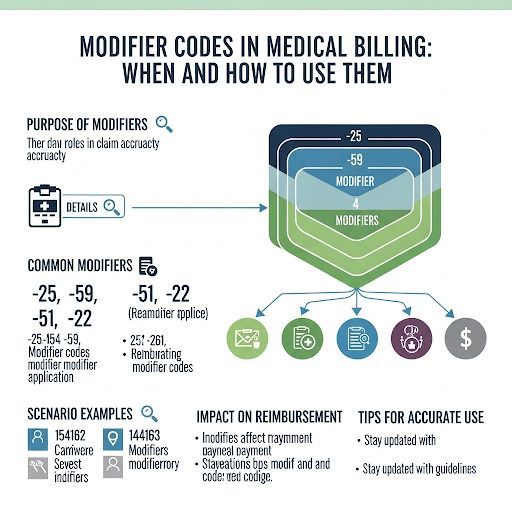
CPT or ICD-10 codes, procedure descriptions
Amount Billed
The provider’s original charge
Allowed Amount
The negotiated rate insurance will pay
Insurance Payment
How much your plan covered
Patient Responsibility
Your copay, coinsurance, or deductible
Remarks/Notes
Additional clarifications or denial reasons
Common Reasons Patients Misunderstand EOBs
Patients often confuse an EOB with a bill because:
- The layout looks like an invoice — with numbers in bold.
- Insurance language can be full of abbreviations and codes.
- It lists an “Amount You Owe” without explaining payment instructions.
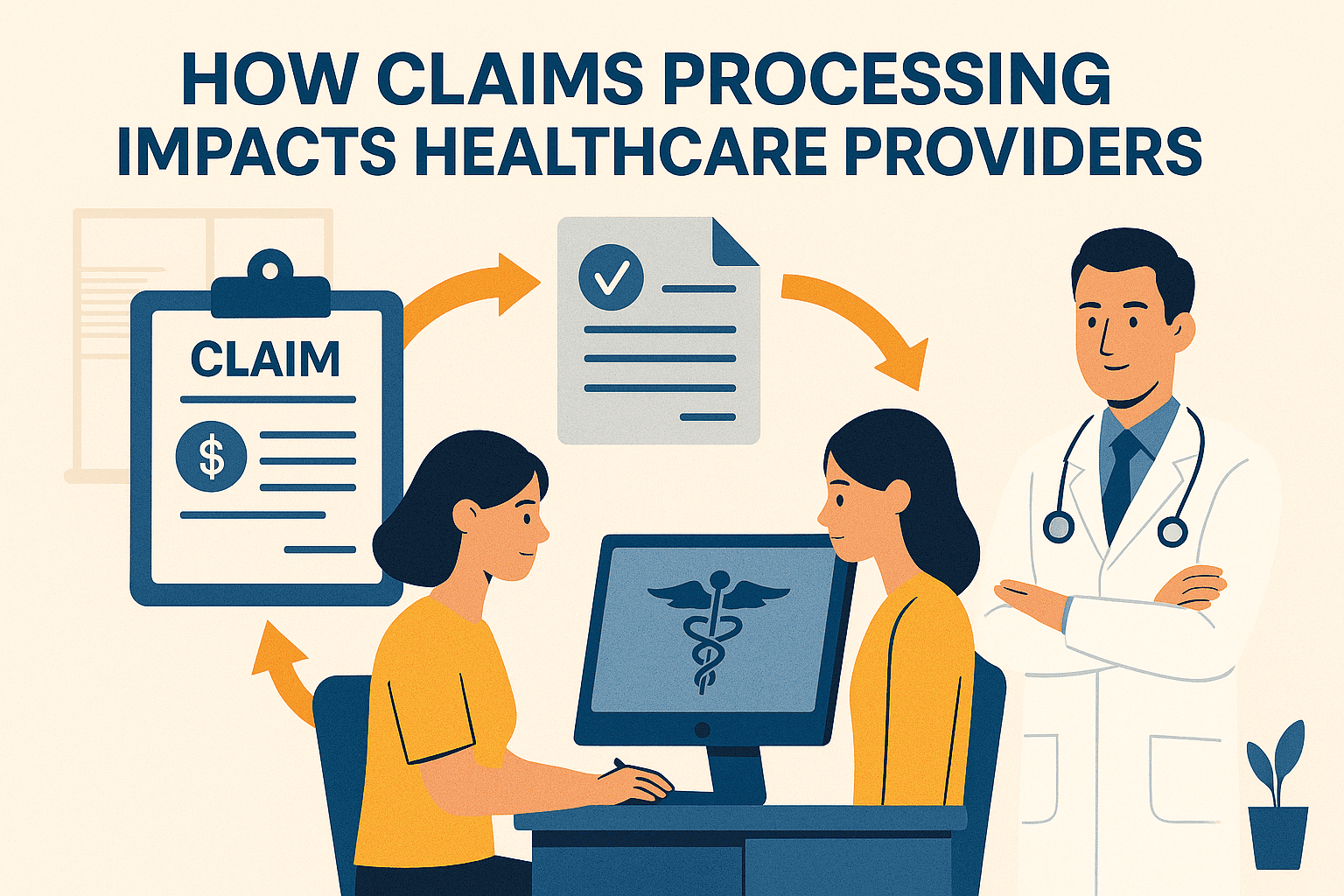
For small practices, unclear EOB explanations can lead to:
- More billing-related phone calls
- Delayed payments from patients
- Frustration that affects patient satisfaction
How Small Practices Can Help Patients Read EOBs
Clear communication about EOBs can improve collections and trust. Best practices include:
- Providing a quick reference guide for reading EOBs
- Highlighting “This is not a bill” in patient communications
- Offering billing consultations for high-cost services
- Using patient portals to link EOBs with billing records
(Related: Medical Billing for Small Practices)
EOB vs. Medical Bill — The Key Difference
EOB
Medical Bill
Sent by insurance company
Sent by provider or billing company
Explains what insurance covered
Requests payment from the patient
Includes codes & claim details
Lists actual amount due
No payment action required
Payment action required
Why EOB Accuracy Matters
A mistake on an EOB can lead to incorrect patient balances or claim denials.
Practices should:
- Verify CPT & ICD-10 codes before claims submission
- Follow up on discrepancies immediately with insurers
- Keep documentation of all communications for appeals
Final Takeaway
An Explanation of Benefits is a valuable tool for both patients and providers — if it’s understood correctly. By helping patients interpret their EOBs, small practices can reduce confusion, speed up payments, and improve overall satisfaction.
If your practice struggles with billing transparency or wants to improve patient payment timelines, outsourcing medical billing can streamline the process and ensure EOB accuracy from the start.