CPT vs ICD-10 Codes: What’s the Difference and Why It Matters for Billing Accuracy
In medical offices across the U.S., one of the most common sources of confusion among staff—especially new admin and billing coordinators—is the difference between
CPT codes and ICD-10 codes. These two types of medical codes serve entirely different purposes, and mixing them up can lead to
claim denials,
billing errors, and
compliance risks.
Whether you're a healthcare provider, front office staff, or billing team member, this guide explains what each code type means, how they work together, and why getting them right is essential—especially if you're billing in states like California, where payer rules can be even more specific.
Why Staff Often Confuse CPT and ICD-10 Codes
Here’s a typical situation in a clinic:
A provider documents a diagnosis and a procedure, and the billing staff must translate that into the right code combination. But:
- A new staff member might use a diagnosis code (ICD-10) where a procedure code (CPT) is required.
- Some claim rejections don’t clearly say what was wrong—just “coding mismatch.”
- Training materials often lump all “codes” together without breaking down use cases.
This coding confusion delays reimbursement, increases workload, and may even flag audits.
CPT Codes vs ICD-10 Codes: Key Differences You Need to Know
Let’s break it down clearly:
1. What Are CPT Codes?
- Stands for: Current Procedural Terminology
- Used for: Procedures and services performed (e.g., office visits, surgeries, tests)
- Maintained by: American Medical Association (AMA)
- Examples:
- 99213 – Office/outpatient visit, established patient
- 71045 – Chest X-ray
- 93000 – EKG
2. What Are ICD-10 Codes?
- Stands for: International Classification of Diseases, 10th Revision
- Used for: Diagnoses (the reason a service was provided)
- Maintained by: World Health Organization (WHO)
- Examples:
- E11.9 – Type 2 diabetes without complications
- J01.90 – Acute sinusitis
- M54.5 – Low back pain
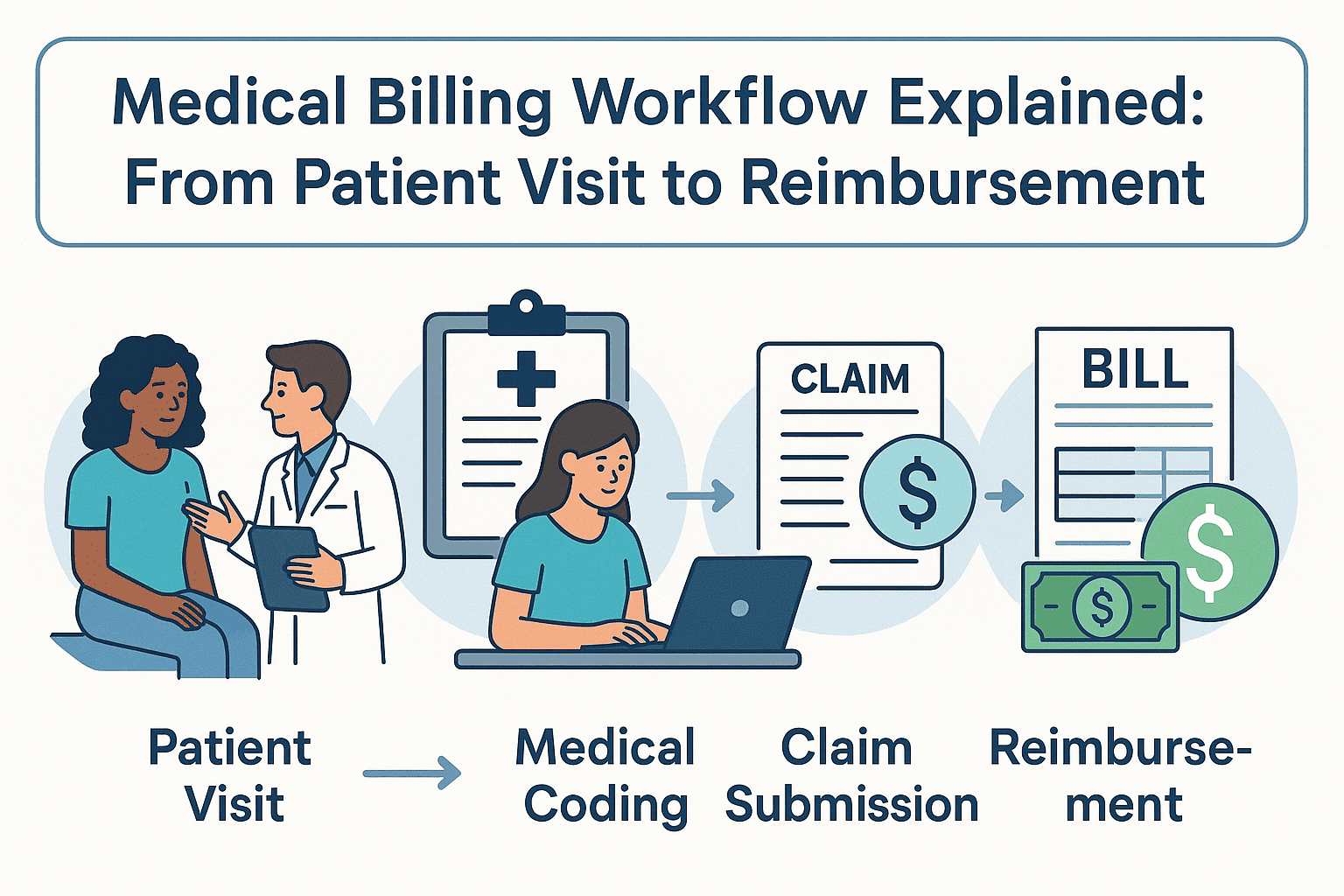
3. CPT Codes = What Was Done | ICD-10 Codes = Why It Was Done
You need both for a clean claim:
- ICD-10 tells the payer why the patient needed care.
- CPT tells them
what care was provided.
If you only include one or mismatch them, the claim may be denied or delayed.
Why This Coding Distinction Matters in California Billing
In states like California, where payer policies vary widely across private insurers, HMOs, and Medi-Cal, accurate coding is even more critical. Errors in CPT/ICD-10 combinations can result in:
- Rejected claims from Anthem, Blue Shield, or Kaiser
- Denied Medi-Cal encounters due to invalid code pairings
- Payment delays due to "unspecified" diagnosis codes
Staff training in
medical billing and coding California guidelines often highlights how stricter regional payer edits increase the need for coding accuracy.
How to Prevent Coding Errors in Your Practice
If your front desk or billing staff struggle to match CPT and ICD-10 codes correctly, here’s how to reduce errors:
- Use coding crosswalk tools that link common ICD-10 codes with typical CPT services.
- Review denied claims monthly to identify recurring coding mismatches.
- Train new staff using real-life claim examples, not just theoretical scenarios.
- Use certified billing partners who stay updated on California-specific coding changes.
FAQs: CPT vs ICD-10 Coding Questions
Can I submit a claim with just an ICD-10 code?
No. A claim must include at least one CPT code to show the service rendered. ICD-10 codes alone explain the diagnosis, not the work done.
What happens if the CPT and ICD-10 codes don’t align?
Misalignment often results in a claim denial with a vague remark code. This means manual rework, delayed payments, and often, patient confusion.
Are CPT and ICD-10 codes updated yearly?
Yes. Both sets are updated annually. CPT codes usually update in January, while ICD-10 codes update in October. Always use the most current versions to avoid denials.
Where can staff learn proper medical coding?
In-house training, AAPC-certified courses, or working with a professional
medical billing and coding California team can provide accurate, ongoing education.
Final Thought
The difference between
CPT codes and ICD-10 codes isn’t just technical—it directly impacts how quickly your clinic gets paid and how smoothly your operations run. Accurate coding reduces denials, protects against audits, and ensures staff confidence when handling claims.
If your clinic is located in a complex payer landscape like California and struggling with staff coding accuracy, it may be time to consult a trusted medical billing and coding California service. The right support team will help you eliminate guesswork and secure faster reimbursements.