Modifier Codes in Medical Billing: When and How to Use Them
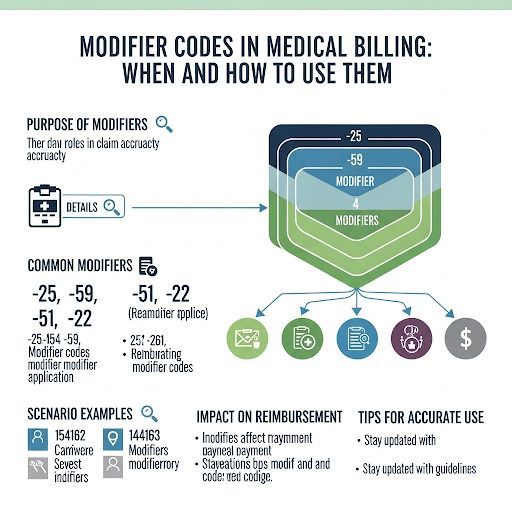
Medical billing is a precise process where even the smallest error can lead to denied claims or delayed payments. Among the most common mistakes is the incorrect use of modifier codes. These two-digit numbers added to CPT or HCPCS codes provide crucial details about the service rendered. When modifiers are missing or misused, providers risk revenue loss, compliance issues, and frustrated patients.
In this article, we’ll explain what modifier codes are, why they matter, and how to use them correctly to ensure smooth claim processing.
What Are Modifier Codes in Medical Billing?
Modifier codes are two-character suffixes (numeric or alphanumeric) attached to CPT or HCPCS codes. They don’t change the procedure itself but clarify how, where, or why it was performed.
For example:
• Modifier 25: Significant, separately identifiable E/M service on the same day as another procedure.
• Modifier 59: Distinct procedural service (used to avoid unbundling issues).
• Modifier 26: Professional component of a service.
Without modifiers, payers may assume a procedure is duplicated, incorrectly bundled, or not medically necessary.
Why Modifier Codes Matter
The correct use of modifiers impacts:
• Reimbursement: Incorrect modifiers often lead to underpayment or complete denial.
• Compliance: Misuse may trigger audits or penalties.
• Patient Experience: Errors cause confusing bills and payment delays.
• Practice Revenue: Missing modifiers can lead to thousands in lost revenue annually.
Commonly Misused Modifier Codes
1. Modifier 25 – Overused for E/M services, often flagged for medical necessity.
2. Modifier 59 – Misapplied to bypass bundling edits, creating compliance risks.
3. Modifier 22 – Used for increased procedural services but requires strong documentation.
4. Modifier 50 – Bilateral procedures, sometimes omitted, leading to reduced payment.
Many denials happen because practices fail to justify the modifier with sufficient documentation.
Best Practices for Using Modifier Codes
To avoid denials and payment delays:
• Verify payer guidelines: Different insurers may interpret modifiers differently.
• Use documentation as proof: Always back modifiers with clinical notes.
• Avoid overuse: Repeated use of 25 or 59 raises red flags with payers.
• Invest in training: Ongoing education for billing staff reduces errors.
• Leverage software checks: Billing systems with claim scrubbing features can catch modifier issues before submission.
Pain Point: Modifiers Missing or Misused
For internal medicine practices, modifier misuse is especially common due to complex patient cases involving multiple services in a single visit. Missing or incorrect modifiers cause delays in reimbursement, straining cash flow. Many practices turn to specialized
Medical Billing Companies Internal Medicine to ensure accurate coding and compliance.
FAQs About Modifier Codes in Medical Billing
1. What happens if I don’t use a modifier when required?
The claim may be denied, underpaid, or flagged for review, delaying reimbursement.
2. Can modifiers affect compliance audits?
Yes. Overusing certain modifiers like 25 or 59 may trigger payer audits for possible abuse.
3. Are modifier rules the same for all payers?
No. Each insurance company may have unique requirements, so it’s essential to verify payer-specific rules.
4. How do I know which modifier to use?
Cross-reference CPT guidelines, payer instructions, and documentation. If unsure, consult a certified coder or billing company.
Final Thoughts
Modifier codes play a critical role in accurate medical billing and coding. When used correctly, they ensure providers are reimbursed fairly for the services they perform. But when modifiers are missing or misused, the consequences can be costly.
Partnering with expert medical billing professionals can help internal medicine practices reduce errors, improve claim acceptance rates, and maintain compliance in today’s complex reimbursement environment.