Medical Billing Companies for Dermatology Are Essential for Practice Efficiency
Medical billing for dermatology practices requires specialized knowledge due to the unique nature of dermatological services. From routine skin exams to complex surgeries and cosmetic treatments, each dermatology procedure must be accurately coded to ensure proper reimbursement. This is where medical billing companies dermatology play a crucial role. By partnering with medical billing companies for dermatology, practices can improve their revenue cycles, reduce errors, and focus on providing exceptional patient care.
The Role of Medical Billing Companies Dermatology in Streamlining Revenue Cycle Management
Dermatology is a complex field, and medical billing for dermatology requires precise knowledge of dermatology-specific codes and payer requirements. Medical billing companies dermatology specialize in these areas, ensuring that claims are accurately submitted and processed. This reduces the likelihood of claim denials or rejections, which can significantly delay reimbursements and affect a practice's cash flow. By outsourcing to medical billing companies dermatology, practices ensure that the revenue cycle is handled by experts who know the intricacies of dermatology billing.
The value of medical billing companies for dermatology extends beyond just accuracy. They help dermatologists navigate the ever-changing landscape of insurance policies, coding rules, and compliance requirements. These companies are dedicated to staying updated on the latest industry trends and payer guidelines, which is critical in minimizing denials and ensuring consistent reimbursement.
Why Dermatology Practices Should Consider Medical Billing Companies Dermatology
Outsourcing medical billing to medical billing companies dermatology offers numerous advantages, especially for dermatology practices seeking to reduce administrative burdens and enhance operational efficiency. Here are some reasons why dermatologists should consider outsourcing to these specialized companies:
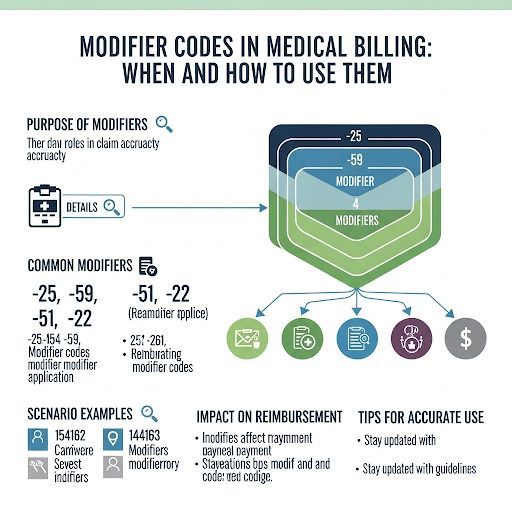
- Expertise in Dermatology Coding: Medical billing companies dermatology are familiar with the complex codes and guidelines specific to dermatology treatments, ensuring proper billing for each procedure. From acne treatments to Mohs surgery, the proper code ensures accurate reimbursement.
- Reduced Claim Rejections and Denials: One of the main benefits of partnering with medical billing companies for dermatology is the reduction in claim denials. These companies have a deep understanding of payer requirements and can handle denials efficiently, increasing the likelihood of successful claims.
- Cost-Effective: Outsourcing medical billing to specialized companies is often more cost-effective than managing billing in-house. Dermatology practices can avoid the costs of hiring, training, and maintaining an in-house billing team, which can save significant resources. This is particularly helpful for medical billing for small practices, where budgets may be tighter.
- Improved Cash Flow: With the help of medical billing companies dermatology, practices experience faster reimbursements and fewer delays in payments. As a result, dermatologists can maintain a healthier cash flow, which is vital for the financial stability of their practices.
The Advantages of Medical Billing Outsourcing for Dermatology Practices
For dermatology practices looking to cut costs without compromising on the quality of their billing services, outsourcing to medical billing companies for dermatology is an ideal solution. Not only does it lower administrative expenses, but it also ensures the accuracy of the claims submitted to insurance companies, which reduces the chances of costly errors.
Additionally, medical billing outsourcing costs are typically lower than maintaining an in-house billing department. This makes it a more viable option for smaller dermatology practices that may not have the resources to invest in full-time billing staff. The flexibility of outsourcing allows practices to scale their services based on patient volume and business needs.
Conclusion: Maximize Efficiency with Medical Billing Companies Dermatology
The decision to partner with medical billing companies dermatology is a smart one for any dermatology practice. These companies bring specialized knowledge, reduce errors, streamline the revenue cycle, and improve overall operational efficiency. Whether you are a small practice or a larger dermatology group, outsourcing medical billing to professionals ensures that your practice remains financially healthy and compliant with ever-evolving insurance regulations.
Valley Medical Billing Services is a company that puts its providers and patients first and foremost. We conduct our services in a courteous, ambitious, and professional manner with enthusiasm, compassion, and a great deal of determination. We aim to prevail in all aspects of the medical billing spectrum. We care about the people we work for and with and want our reputation to surpass the rest! Contact us today to discuss how we can enhance your dermatology practice’s billing process and ensure you can focus on providing the best care for your patients.